Mini-residency in geriatrics emphasizes team care model of older adult oral health
A unique School of Dentistry Continuing Dental Education course supported by the Minnesota Department of Health is giving dental providers insight into the interprofessional nature and value of specialty geriatric care.
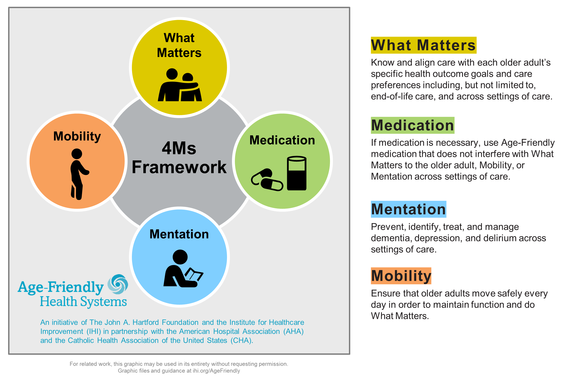
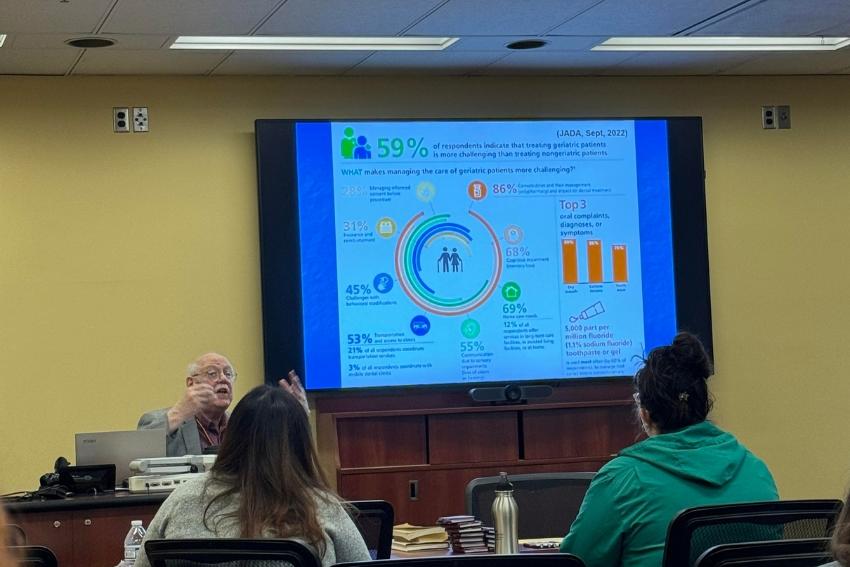
A four-day, 32-hour program, “Mini-residency in Geriatrics and Long-term Care for the Dental Team” invites providers to explore a variety of topics key to effectively caring for older patients who have more complex needs. The course has been active for over 30 years and focuses on topics related to the “4 Ms” for age-friendly health care: mobility, medications, mentation/mood and what matters—ensuring older adults receive the care they want and need.
“Working with older adults can be complex,” explained Stephen Shuman, DDS, MS, FGSA, professor and director of the Division of Hospital and Special Care Dentistry and director of the Oral Health Services for Older Adults (OHSOA) Program, who developed the mini-residency with his colleagues. “Older adults may have a variety of health concerns or functional issues and live in a variety of settings, from independent housing, to home health support, to assisted living to nursing homes or hospice. Long-term care is now a spectrum of options, and to effectively care for these folks, you’ve got to figure out how to work in those systems. That’s not something dental professionals typically learn much about in school.”
A team sport
When Shuman first created this program, he knew that providing good geriatric care was not something clinicians could do by themselves—nor could he do the mini-residency alone. “We like to say that good geriatric care is a team sport,” he explained. “You can’t do it by yourself.”
Shuman has always enlisted members of the interprofessional teams he has worked with at the OHSOA community clinics to help teach the course and is now drawing on the expertise of his U of M geriatrics colleagues from the HRSA-funded Minnesota Northstar Geriatrics Workforce Enhancement Program based in the Medical School, including Benjamin Rosenstein, MD, MA, assistant professor and geriatrician in the Department of Family Medicine and Community Health, and Sharon Kimble, PT, DPT, director of the Geriatric Residency in the Division of Physical Therapy at the University of Minnesota Medical School.
Rosenstein “provided a discussion about the background and role of a geriatrician and how we can be partners in the care of older adults,” including an overview of medical issues providers may encounter with older patients.
“This was a good opportunity to interact with dental providers who wish to learn more about care of older adults,” he reflected. “As someone who provides care in long-term care settings, I was also able to discuss the complexities and needs of that population.”
Rosenstein echoed Shuman’s sentiment about the need for interprofessionalism in geriatric care. “We are often working with some of the most medically complex people with the added complexity of geriatric syndromes, in addition to complex social needs,” he said. “Providing the best care often requires more than one person and more than one area of expertise.”
Kimble invited physical therapy graduate students from the Class of 2026 to help her run a lab, teaching participants how to manage wheelchairs, walkers, sliding boards and other methods of helping older adults in and out of the dental chair. “Physical therapists are well-suited to teaching this content and the decision making that goes along with how to assist patients or clients who are not fully mobile,” she explained.
“The mini-residency participants were enthusiastic learners and grateful to have an expert at their disposal to ask many pertinent questions, and the physical therapy students did a great job demonstrating on-their-feet thinking and problem solving,” Kimble reflected.
The teamwork this group of providers displayed comes from their firsthand experience working together. “We’re sort of teaching by example,” Shuman explained. “Geriatric care providers have been through many clinical scenarios and real-life situations that we can share with the participants to model these interactions. Going through those experiences together gives us a shared history, which opens participants’ eyes to the kinds of things that can happen and how to best manage them.”
That shared history includes issues such as falls, eloping patients, confused drivers and many other instances of specialized geriatric care that allow participants to learn by example. “They can learn from our real clinical cases and experiences.,” Shuman said.
Expanding the team
New to the mini-residency this year was a focus on encouraging rural providers to participate, thanks to a grant from the Minnesota Department of Health’s (MDH) Oral Health Program. Like most states, the concentration of older adults living in rural Minnesota communities is higher than in urban areas. MDH’s HRSA-funded “Grants to States to Support Oral Health Activities” is now focused on promoting age-friendly oral health care throughout the state and provided funds for six rural Minnesota providers to attend the mini-residency program and implement what they learned at their own practices.
“Attending the mini-residency as a new State Oral Health Director in 2017 was instrumental in helping me envision an age-friendly dental public health system in Minnesota,” said Prasida Khanal, BDS, MPH, State Oral Health Director at the Minnesota Department of Health. “Thanks to the Health Resources and Services Administration (HRSA) funding, the Minnesota Department of Health provided 6 scholarships for the mini-residency. We wanted to recognize dental professionals serving in Dental Health Professional Shortage Areas and equip them with the skills necessary to meet the unique needs of older adults, ensuring comprehensive and age-friendly oral health care.”
Robert Lew, DDS, adjunct dentist at Hibbing Community College Dental Clinic, said these funds “made all the difference” in allowing him to attend the mini-residency.
The residency was “an excellent learning experience” for Lew, who “learned much useful information which will help improve my care for geriatric patients.” In particular, he appreciated learning more about “the special considerations necessary for the arrangement of care for the geriatric population.”
Rosemary Skriver, BSDH ’22 MDT ’23, also credits the scholarship funds for her decision to attend the mini-residency. “As a provider from rural northern Minnesota, the opportunity for continuing education in a formal interactive format is hard to come by,” she explained. “The funds certainly allowed me to feel more comfortable taking time away from the office.”
Skriver, who has already seen the impact aging has on her patients, sees this course as very valuable for her future as a provider. “I know that as my patients continue to age, I will need to find ways to adapt to provide better care,” she said. “This course gave me the foundational knowledge to make adjustments to how I practice dentistry and individualize treatment to the needs of each patient.”
She is particularly looking forward to implementing new insights in treatment planning, and to sharing this new knowledge with her team, “so that we can incorporate some key aspects for providing safe and effective care, allowing us to better serve our elderly patients.”
These takeaways are exactly what Shuman and his colleagues hope will come out of the course: a renewed outlook on an interprofessional, multi-dimensional understanding of geriatric care. If such care is a “team sport,” as Shuman calls it, this mini-residency helped his team grow by 17 more players.