Dentistry, Engineering Researchers explore COVID-19 Spread and Safety in Dental Offices
A collaborative effort between University of Minnesota researchers and clinicians made a real-life, immediate impact on patient care and safety amid the COVID-19 pandemic.
“Without this expertise, I don’t believe our clinics would have opened up as soon as they did,” said Paul Olin, DDS, MS, Interim Associate Dean for Clinical Affairs at the University of Minnesota, of the project.
 It all started in March 2020, when Governor Tim Walz halted all non-emergency dental procedures, effectively shutting down most of the School of Dentistry’s clinical presence. “In some respects, that did us a favor,” said Olin: it allowed him to take a step back and think through the risks of what he’d begun to suspect was an airborne pathogen.
It all started in March 2020, when Governor Tim Walz halted all non-emergency dental procedures, effectively shutting down most of the School of Dentistry’s clinical presence. “In some respects, that did us a favor,” said Olin: it allowed him to take a step back and think through the risks of what he’d begun to suspect was an airborne pathogen.
Olin connected with other faculty, including:
- Paul Jardine, PhD, a professor of diagnostic and biological sciences,
- Rachel Uppgaard, DDS, assistant clinical professor of oral and maxillofacial surgery,
- John Madden, CDT, Allied Healthcare Professional,
- Brent Larson, DDS, MS, director of orthodontics and professor of developmental and surgical sciences, and
- Jeremy Anisman, PhD, molecular virology researcher.
The team began to tackle a series of questions together: how does the COVID-19 virus spread throughout a dental office? What tools make that spread worse? And what can we do to protect ourselves and our patients?
The researchers brought their unique areas of expertise to the table and engaged in a study of particle spread. Jardine works with bacteriophages, viruses that are harmless to humans but infect bacteria. “When Dr. Olin approached me, he asked the perfect question,” Jardine explained. “It’s not about the viruses I work with, but what you can use them for—he asked if I could use them to test aerosols.”
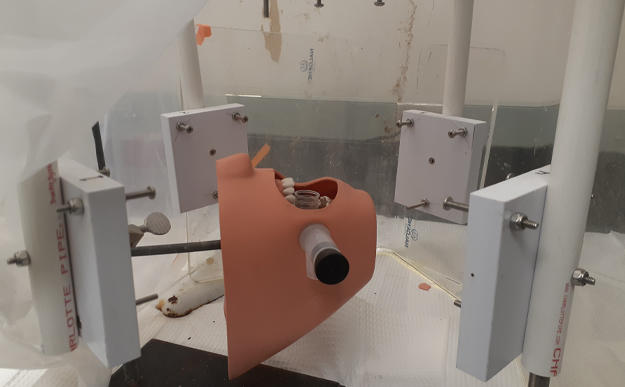
Jardine, Olin, and their team produced a model to safely aerosolize Jardine’s virus particles using a nebulizer and test their spread throughout the room. Early work focused on whether various suction devices and air filtration units could effectively capture aerosols that could carry virus. When that worked, the team paired up with Judy Danielson, MDH, clinical professor of developmental and surgical sciences in periodontology, and began working with mannequins to see how various dental procedures impacted the generation and spread of aerosols.
“One of the biggest questions we had in dentistry at the time was when and how people could start using particular tools,” Olin explained. The team tested high- and low-speed handpieces, cavitrons, and other dental procedures to determine how an aerosol might spread.
 To further understand how those aerosols might move throughout the room and possibly infect individuals, as well as how devices like a vacuum or HEPA filter might stop that spread, the team worked with Gary Anderson, DDS, MS, a professor of developmental and surgical sciences who studies clinical measurement, and School of Engineering faculty, including Qisheng Ou, PhD, Jiarong Hong, PhD, David Nedrelow, PhD, and David Pui, PhD. The team oversaw optical imaging through digital inline holography and laser sheet imaging to explore how devices like a saliva ejector, a high-volume extractor, or an extraoral local extractor might reduce the risk of infection.
To further understand how those aerosols might move throughout the room and possibly infect individuals, as well as how devices like a vacuum or HEPA filter might stop that spread, the team worked with Gary Anderson, DDS, MS, a professor of developmental and surgical sciences who studies clinical measurement, and School of Engineering faculty, including Qisheng Ou, PhD, Jiarong Hong, PhD, David Nedrelow, PhD, and David Pui, PhD. The team oversaw optical imaging through digital inline holography and laser sheet imaging to explore how devices like a saliva ejector, a high-volume extractor, or an extraoral local extractor might reduce the risk of infection.
They found that an extraoral local extractor did the best job of decreasing spread while also being fairly simple to use. Moving forward, the team hopes to continue examining the level of protective equipment they’ve recommended and secure publication for their manuscript on the study.
“Without this expertise, I don’t believe our clinics would have opened up as soon as they did,” Paul Olin, DDS, MS, Interim Associate Dean for Clinical Affairs.
Olin, Jardine, and Anderson are proud of how this project not only made a real impact on the School of Dentistry’s clinics, but also how it brought together researchers whose areas rarely converge.
“We’re two extremes,” explained Jardine. “Dr. Olin and Dr. Anderson are very clinically focused. For me, most of the people I talk to on a daily basis are structural biologists and biophysicists.”
“As a school, we have this really broad diversity,” he continued. “In times like these, it provides incredible opportunities.”
 Olin agreed, noting that Jardine’s expertise was crucial to making patient-facing decisions. “The only way I could justify the purchase of the mitigation devices I did, and that they would work, was to work with Dr. Jardine to test them.”
Olin agreed, noting that Jardine’s expertise was crucial to making patient-facing decisions. “The only way I could justify the purchase of the mitigation devices I did, and that they would work, was to work with Dr. Jardine to test them.”
For Anderson, the experience reflected the root of impactful research. “There was a real practical question we were wrestling with: how do we make sure we’re safe? How do we know when we’ve done enough?” The ability to bring engineers, basic scientists, and clinicians together to answer that question was “pretty astounding.”
And it was a remarkable experience in problem solving—one that gave the researchers hope. “I typically expect the investment of my work to pay off in ten to twenty years,” said Jardine. “This ability to work with people from different skill sets and focus on a critical issue with clinical faculty who took charge of the situation was really exciting.
I’m very proud of our school, because of how we responded so effectively and quickly, with full dedication to our mission: to provide the safest environment we can for our patients and staff.”
A shorter version of this piece previously appeared in the American Dental Education Association’s Bulletin of Dental Education.